Liver cirrhosis: An Overview of Diagnosis and Management Approach
Ahmed Saleh K Almarhoun, Abdullah Ahmed Aladnani, Haneen Ahmad Khouja, Mohamed Hussien Elzinkarani, Mohamad Metab Alenazi, Laila Taher Alaswad, Mahdi Farah A Alanazi, Atif Mohammed Hakami, Mohrah Abdulaziz Alyabis, Yasser Owaidh Alsahli*
Abstract
Background: Liver cirrhosis is one of the most common complaints in the medical field. Many causes are identified to cause liver cirrhosis, such as alcohol, infections, or genetic causes. Many modalities can help in the diagnosis of liver cirrhosis, however, biopsy still the gold standard. Many complications can be a result of liver cirrhosis, portal hypertension is a common complication which needs to be identified and treated as early as possible. Treatment mainly depends on the cause, if the cause could be treated early, the liver injury could be reversed, and otherwise, it will be permanent and can be fatal. Objective: The objective of this review is to discuss Liver cirrhosis, pathophysiology, investigations, complications, and treatment in a general view. Method: We searched the PubMed database looking for relevant articles to the topic using Mesh terms, “liver cirrhosis ". Conclusion: Many causes are identified to cause Liver cirrhosis, for that, early detection of the cause and proper treatment could prevent liver cirrhosis and it is complications.
Keywords: Liver Cirrhosis, chronic liver disease, portal hypertension, Hepatic Encephalopathy, liver biopsy.
Introduction
liver cirrhosis, or as it is called end-stage liver disease, is characterized by diffuse regenerated liver parenchymal cell nodules separated by fibrous septa, and this will lead to disturbing in liver architecture and thus failing of liver synthetic functions such as proteins and coagulation factor (Figure 1) (Tsochatzis et al., 2014). Liver cirrhosis usually is a complication or end-stage of liver diseases such as Hepatitis B and C virus, or excessive intake of alcohol, which will turn into cirrhosis after years if left untreated or not stopped alcohol drinking (Tsochatzis et al., 2014). Liver transplantation is the most appropriate curative treatment if liver cirrhosis is completed (Hassankhan et al., 2020; Elsheikh et al., 2020; El Faizy, 2019; Ibrahim and Abdelbasset, 2020). There are no ways to reverse or regress the abnormal architecture of the liver after its disturbing, and this is the most difficult thing in the treatment or management plan of liver cirrhosis (Tsochatzis et al., 2014). This review will discuss the epidemiology of liver cirrhosis, pathophysiology, pathology, complications, and management.
Epidemiology:
Cirrhosis is the 14th most common cause of death worldwide; it increases morbidity and mortality, but it is the 4th in central Europe (Blachier et al., 2013). It results in 1.03 million deaths per year all over the world; cirrhosis is the main cause of liver transplantation. It caused 5500 liver transplantation surgeries approximately per year (Lozano et al., 2012). It is more common in developed countries due to an increased chance of infection in hepatitis C and hepatitis B it is usually explained by the hygiene hypothesis; infection of hepatitis B is more common in sub-Saharan African and Asia (Lozano et al., 2012). The prevalence of the disease is hard to be calculated because the initial stages of the disease are asymptomatic, so it is very hard to detect (Lozano et al., 2012).
Discussion
Pathophysiology:
Liver cirrhosis comes usually after liver steatosis (fatty liver) or hepatitis –the cirrhosis can be stopped or reversed during those steps- if the cause is resolved in these stages and does not proceed to fibrosis or scar tissue formation and nodular regeneration of hepatic lobules, this scar tissue will not lead to blockage of the blood vessels and then will not cause portal hypertension which will be discussed more in complication part (Suva, 2014). The main cells that play a role in the formation of the cirrhosis are Ito cells (stellate cells) – the main function of those cells is the storage of Vitamin A-, this type of cells are found in the space of Disse, any inflammation or hepatic parenchymal cell damage can lead to activation of stellate cells and make them secretes collagen and fibrous to obstruct the space of Disse as well as the blood vessels (Suva, 2014). If the formation of the fibrous septa has been completed the hepatic lobules will be separated from each other and this will lead to the formation of regenerating nodules and failing of liver normal functions such as synthesizing of proteins and coagulation factors in addition to carbohydrates metabolism (Suva, 2014).
Some researchers have been conducted to show that the Kupffer cell (liver macrophages) also has a very important role in secreting collagen and forming the fibrous septa in addition to the stellate cells (Duffield et al., 2005). The stellate cells can be activated by various triggering factors such as inflammatory cytokines or ROS –reactive oxygen species – which then activate autocrine and paracrine receptors on the surface of Ito cells (stellate cells) to increase its releasing of collagen fibers at the beginning of disease stage swollen stellate cells can be noticed in addition to the loss of retinoid (Vitamin A) with increase sensitivity to fibrogenic and proliferative cytokines, e.g., TGH-B1 (transforming growth factor-beta), and PDGF (platelet-derived growth factor), and up-regulation of these receptors (Puche et al., 2011). Increasing of inflammatory cytokine release will cause increasing of collagen type I and III secretions by disturbing the balance mechanism between the MMP (matrix metalloproteases), which destruct the collagen and fibrous tissue, and TIMPs (tissue inhibitor of metalloproteases), which stop the destruction of collagen fibers, so in the stage of liver cirrhosis increase activation of TIMP and decrease, or loss of function in MMP will be noticed, and this is the underlying cause behind increasing and formation of fibrous septa (Puche et al., 2011).
In the initial stages of liver disease, this fibrosis can be reversible if not completed by treating the underlying cause such as viral hepatitis or excessive alcohol drinking. The most important pathological features of liver cirrhosis are regenerating nodules separated by fibrous septa and disturbance of liver architecture and this will lead to a decrease in liver blood flow and stenosis of the portal system by fibrous tissue, which causes portal hypertension and its complication, there are three morphological types of nodules: a) Micronudular cirrhosis, the size of regenerating nodules is less than 3 mm, and it involves the whole liver; usually, the cause of micronodular cirrhosis is alcohol intake , which induces hepatocellular injury, b) Macronodular cirrhosis, the size of regenerated nodules is more than 3 mm, and it is usually caused by chronic viral hepatitis, c) mixed nodular cirrhosis, the nodules are mixing some less than 3 mm and some more than this (Suva, 2014). Macroscopic picture of the liver: in the initial stages of enlarged liver cab noticed, then liver shrinkage occurs with the irregular liver surface (Suva, 2014).
The complication of liver cirrhosis:
The most important liver cirrhosis complication is portal hypertension which is caused by the narrowing of portal systems by the fibrous tissue, portal system hypertension is defined by HVPG (is the pressure difference between the portal vein and the inferior vena cava) more than 5 mmHg (Groszmann et al., 2005). There are mainly 3 complications that arise from portal hypertension: hemorrhoids, Caput Medusa, and esophageal varices this article will focus on the esophageal varices since it is the most dangerous complication. Esophageal varices developed when the HVPG is more than 10 mmHg the collateral circulation opened and esophageal varices occur it is very prone to rupture and bleeding so hematemesis can be present in the patient complaint (Groszmann et al., 2005). Esophageal varices indicate stage 2 clinical cirrhosis and it is the most common cause of death in liver cirrhosis patients (de Franchis, 2010). As a result, prophylactic treatment is required and the most effective prophylactic treatment is a non-selective B blocker which decreases the HVPG by 20% (Abraldes et al., 2003). Add to that, there is a surgical procedure called endoscopic band ligation both show a significant decrease in the mortality rate (Burroughs et al., 2010). Also, there is an approach called TIPS (transjugular intrahepatic portosystemic shunt) is one of the possible treatments for portal hypertension. This technique can be used in emergency cases, however, it is difficult to be done since it needs a specialized center to do it (García-Pagán et al., 2010).
Ascites, it is defined as an accumulation of fluid in the peritoneal cavity it is caused by portal system hypertension and vasodilation in the splanchnic vessels due to increased synthesis of nitric oxide NO (Wiest and Groszmann, 2002); it is also related to the increasing level of vasoconstrictor in systemic circulation and ant diuretic hormone and RAAS system (rennin, angiotensin, aldosterone) which causes water and sodium retention (García-Pagán et al., 2012). Propranolol has shown a significant effect on the prevention of ascites by lowering the HVPG by 10% (Hernández-Gea et al., 2012). This alteration in circulation can lead to hepatorenal syndrome which indicates end-stage liver disease and causes a mortality rate by 50% within a month (Fede, 2012). The most effective treatment of large volume ascites (i.e 5 litters) is paracentesis (Tsochatzis et al., 2014).
Encephalopathy is caused by a decrease of ammonia excretion and an increase in its precipitation in the brain and central nervous system due to failure of the urea cycle in the liver; it occurs in an advanced stage of liver disease and has a high mortality rate of 64% within a year (Jepsen et al., 2010). Lactulose has shown a significant role in the prevention of this condition as well as Rifaximin, it reduces the risk of recurrence from 46% to 21% (Bass et al., 2010).
Hepatocellular carcinoma is a very dangerous complication of cirrhosis that can occur in any stage of the disease at any time and from any cause. It is fatal since it is a cancer of the liver which can be metastasized into any place of the body, for which, 6-month recurrent ultrasound screening of hepatocellular carcinoma is a very crucial step to prevent or treat the condition in it is early stage (Davila et al., 2011).
Imaging and liver biopsy:
Imaging techniques are not the gold standard in diagnosing liver cirrhosis since they have low sensitivity but high specificity, so it is usually used to exclude liver cirrhosis complication such as hepatocellular carcinoma and portal hypertension, enlarged caudate lobule, splenomegaly, and collateral veins abnormalities are the main things that we search about in the imaging techniques, so the main radiological purpose is to exclude the complication of liver cirrhosis (Martínez-Noguera et al., 2002). Ultrasonography gives very important information about liver architecture, and it is not expensive , and it is available. The most important use of ultrasonography is detecting and screening for portal hypertension, and vessel patency (Schuppan and Afdhal, 2008). Helical CT scans and MRI with contrast are not significantly used to determine the severity of liver cirrhosis, but they are very sensitive in detecting hepatocellular carcinoma and vascular abnormalities (Ito et al., 1999). MRI has a higher sensitivity in detecting those lesions than CT scan, and it is also used to determine the iron load in the liver for hemochromatosis disease detection and liver steatosis (Burrel et al., 2003). The gold standard in diagnosing liver cirrhosis is liver biopsy, so the pathologist can see the disturbing of the liver architecture and regenerating nodules that are separated by fibrous septa so the assessment of risk progression can be determined (Schuppan and Afdhal, 2008). The biopsy can be taken either by radiological guided percutaneous or by laparoscopic route (Schuppan and Afdhal, 2008). Sometimes the conformational of the diagnosis by the biopsy is not required since the clinical presentation is so indicative of liver cirrhosis (Schuppan and Afdhal, 2008).
Treatment and liver transplantation:
The treatment of liver cirrhosis depends on the treatment of the underlying disease, so in a patient with liver cirrhosis due to excessive alcohol intake, the patient must stop drinking alcohol, and this can treat or reverse the liver cirrhosis if the steps did not complete. In patients with HCV (hepatitis C virus), the patient should be treated by interferon so viral eradication is one of the most important steps in preventing or treating liver cirrhosis (Everson, 2005). On the same page, patients with HBV (hepatitis B virus) should be treated with Lamivudine, and this shows a 50% decreasing probability of causing liver cirrhosis after viral eradication (Schuppan and Afdhal, 2008).
Liver transplantation is the only curative treatment in a patient with end-stage liver disease that cannot be treated in an alternative way, and it shows a survival rate of 83% within a year, 70% for five years survival rate and 61% survival rate for eight years, there are still some challenges in case of liver transplantation such as the immune rejection cases but nowadays it is a rare condition due to the improvement of the immunosuppressive regimen (Roberts et al., 2004).
Conclusion:
Liver cirrhosis is a fatal condition if left to improve with no intervention. It is characterized by regenerative nodules separated by fibrous septa and loss of normal liver architecture. Liver cirrhosis is a complication of chronic liver diseases such as excessive alcohol intake, HBV, and HCV. The gold standard diagnosing is a liver biopsy, and the treatment depends on the treatment of the underlying cause or liver transplantation. The most common complication of liver cirrhosis is portal hypertension, and the most dangerous are esophageal varices and hepatocellular carcinoma.
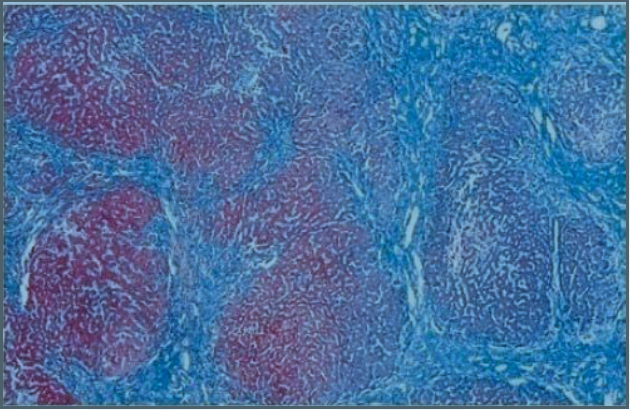
Figure 1: Microscopic appearance of Liver Cirrhosis..
Abraldes, J. G., Tarantino, I., Turnes, J., Garcia‐Pagan, J. C., Rodés, J., & Bosch, J. (2003). Hemodynamic response to pharmacological treatment of portal hypertension and long‐term prognosis of cirrhosis. Hepatology, 37(4), 902-908.
Bass, N. M., Mullen, K. D., Sanyal, A., Poordad, F., Neff, G., Leevy, C. B., ... & Teperman, L. (2010). Rifaximin treatment in hepatic encephalopathy. New England Journal of Medicine, 362(12), 1071-1081.
Blachier, M., Leleu, H., Peck-Radosavljevic, M., Valla, D. C., & Roudot-Thoraval, F. (2013). The burden of liver disease in Europe: a review of available epidemiological data. Journal of hepatology, 58(3), 593-608.
Burrel, M., Llovet, J. M., Ayuso, C., Iglesias, C., Sala, M., Miquel, R., ... & Brú, C. (2003). MRI angiography is superior to helical CT for detection of HCC prior to liver transplantation: an explant correlation. Hepatology, 38(4), 1034-1042.
Burroughs, A. K., Tsochatzis, E. A., & Triantos, C. (2010). Primary prevention of variceal haemorrhage: a pharmacological approach. Journal of hepatology, 52(6), 946-948.
Davila, J. A., Henderson, L., Kramer, J. R., Kanwal, F., Richardson, P. A., Duan, Z., & El-Serag, H. B. (2011). Utilization of surveillance for hepatocellular carcinoma among hepatitis C virus–infected veterans in the United States. Annals of internal medicine, 154(2), 85-93.
de Franchis, R. (2010). Revising consensus in portal hypertension: report of the Baveno V consensus workshop on methodology of diagnosis and therapy in portal hypertension. Journal of hepatology, 53(4), 762-768.
Duffield, J. S., Forbes, S. J., Constandinou, C. M., Clay, S., Partolina, M., Vuthoori, S., ... & Iredale, J. P. (2005). Selective depletion of macrophages reveals distinct, opposing roles during liver injury and repair. The Journal of clinical investigation, 115(1), 56-65.
Roshdy, S. H. A., El- Nahas, N. G., Abd el Aziz Abd el Hady, A., El Faizy, M. W. (2019). Impact of early pulmonary rehabilitation on post liver transplantation. Journal of Advanced Pharmacy Education & Research| Apr-Jun, 9(2),7-12..
Elsheikh, A. M., Teama, M. I., Afify, A. F., Abowarda, M. H., & Almassry, H. N. (2020). Comparative study between conventional trans-arterial chemoembolization (TACE) and drug eluting bead TACE regarding tumour response and liver function tests. Archives of Pharmacy Practice, 11(1), 153-162.
Everson, G. T. (2005). Management of cirrhosis due to chronic hepatitis C. Journal of hepatology, 42(1), S65-S74.
Fede, G. (2012). D ́Amico G, Arvaniti V, Tsochatzis E, Germani G, Georgiadi D, et al. Renal failure and cirrhosis: A systematic review of mortality and prognosis. J Hepatol, 56, 810-8.
García-Pagán, J. C., Caca, K., Bureau, C., Laleman, W., Appenrodt, B., Luca, A., ... & Bosch, J. (2010). Early use of TIPS in patients with cirrhosis and variceal bleeding. New England Journal of Medicine, 362(25), 2370-2379.
García-Pagán, J. C., Gracia-Sancho, J., & Bosch, J. (2012). Functional aspects on the pathophysiology of portal hypertension in cirrhosis. Journal of hepatology, 57(2), 458-461.
Groszmann, R. J., Garcia-Tsao, G., Bosch, J., Grace, N. D., Burroughs, A. K., Planas, R., ... & Gao, H. (2005). Beta-blockers to prevent gastroesophageal varices in patients with cirrhosis. New England Journal of Medicine, 353(21), 2254-2261.
Hassankhan, B., Yaghmaei, P., Parivar, K., & Ebrahim-Habibi, A. (2020). Effect of Beta-adrenergic blockade in High-fat-induced nonalcoholic fatty liver disease. Archives of Pharmacy Practice, 11(2), 87-95.
Hernández-Gea, V., Aracil, C., Colomo, A., Garupera, I., Poca, M., Torras, X., ... & Villanueva, C. (2012). Development of ascites in compensated cirrhosis with severe portal hypertension treated with β-blockers. American Journal of Gastroenterology, 107(3), 418-427.
Ibrahim, A. A., & Abdelbasset, W. K. (2020). The role of physical exercise in treating people with non-alcoholic fatty liver disease. Journal of Advanced Pharmacy Education & Research| Apr–Jun, 10(2), 64-70.
Ito, K., Mitchell, D. G., Hann, H. W., Kim, Y. O. N. G., Fujita, T., Okazaki, H., ... & Matsunaga, N. (1999). Viral-induced cirrhosis: grading of severity using MR imaging. AJR. American journal of roentgenology, 173(3), 591-596.
Jepsen, P., Ott, P., Andersen, P. K., Sørensen, H. T., & Vilstrup, H. (2010). Clinical course of alcoholic liver cirrhosis: a Danish population‐based cohort study. Hepatology, 51(5), 1675-1682.
Lozano, R., Naghavi, M., Foreman, K., Lim, S., Shibuya, K., Aboyans, V., ... & AlMazroa, M. A. (2012). Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. The lancet, 380(9859), 2095-2128.
Martínez-Noguera, A., Montserrat, E., Torrubia, S., & Villalba, J. (2002, February). Doppler in hepatic cirrhosis and chronic hepatitis. In Seminars in Ultrasound, CT and MRI (Vol. 23, No. 1, pp. 19-36). WB Saunders.
Puche, J. E., Saiman, Y., & Friedman, S. L. (2011). Hepatic stellate cells and liver fibrosis. Comprehensive Physiology, 3(4), 1473-1492.
Roberts, M. S., Angus, D. C., Bryce, C. L., Valenta, Z., & Weissfeld, L. (2004). Survival after liver transplantation in the United States: a disease‐specific analysis of the UNOS database. Liver transplantation, 10(7), 886-897.
Schuppan, D., & Afdhal, N. H. (2008). Liver cirrhosis. The Lancet, 371(9615), 838-851.
Suva, M. A. (2014). A Brief Review on Liver Cirrhosis: Epidemiology, Etiology, Pathophysiology, Symptoms, Diagnosis and Its Management. Inventi Rapid: Molecular Pharmacology.
Tsochatzis, E. A., Bosch, J., & Burroughs, A. K. (2014). Liver cirrhosis. The Lancet, 383(9930), 1749-1761.
Wiest, R., & Groszmann, R. J. (2002). The paradox of nitric oxide in cirrhosis and portal hypertension: too much, not enough. Hepatology, 35(2), 478-491.