Surgical Treatment of Patients with Severe Acute Pancreatitis
Samara M.*, Klimov A.E., Persov M.Yu., Kirtadze D.G., Barkhudarov A.A.
Abstract
The aim is to study the clinical profiles of patients with severe AP treated surgically during their stay in the hospital. Methods and materials: a result analysis of treating 125 patients with severe forms of acute pancreatitis was carried out. All patients in the preoperative period were imaged through ultrasound scanning (hereinafter referred to as the US). 40 patients were also imaged through computed tomography (hereinafter referred to as CT). US and CT data obtained before surgery were compared with intraoperative ones. Results: All patients were operated on. Operation indications involved: peritonitis clinical picture in 117 patients (93.6%), arosive vessel bleeding in the necrotizing and sequestrum area in 4 patients (3.2%), jaundice growth in 4 patients (3.2%). 80 patients showed infected pancreonecrosis, 80 patients showed retroperitoneal tissue disease. 34 patients died. Factors affecting the disease outcome were revealed: infected pancreonecrosis, retroperitoneal tissue disease, cachexia, obesity, alcoholism, coronary heart disease, arterial hypertension and hepatic disorders, total ASSES scores are higher than 13 upon admission and before surgery, as well as higher than 16 on the 1st-2nd and 3rd-4th day after the operation. Conclusion: The complex use of computed tomography and ultrasound when diagnosing severe forms of acute pancreatitis increases the informational value of these methods to almost 100%.
Key words: Acute pancreatitis, retroperitoneal tissue, disease outcome prediction
Introduction
In the overall structure of acute surgical abdominal diseases, acute pancreatitis (hereinafter referred to as AP) is the third in incidence after acute appendicitis, and acute cholecystitis (Mohamed and Badr, 2019; Kanjikar, 2019; Haghighi-Morad et al., 2018; Nazarenko et al., 2019; Leppäniemi et al. 2019). Over the past 10 years, the results of acute pancreatitis treatment have slightly improved, but the total rate of deaths arising from its destructive forms and retroperitoneal tissue abnormalities is still up to 70% (Kopchak et al., 2009; Tolstoy et al., 2003).
The present understanding is that the course and prognosis of acute pancreatitis largely depend not only on the volume of pancreatic damage but also on pathological retroperitoneal space changes. The term "para pancreatitis" has been introduced into modern pancreatology, which implies a pathological retroperitoneal tissue process (primarily peripancreatic), develops in patients with acute pancreatitis (Kopchak et al., 2009; Tolstoy et al., 2003; Babi and Momot, 2000).
Although instrumental pancreas and retroperitoneal tissue imaging have significantly improved, which made it possible to determine the disease severity and evaluate its course in real-time mode, the current aspects of diagnosis and complex AP treatment are inconclusive and rather contradictory regarding the criteria for conservative therapy effectiveness, criteria for the time and scope of surgical interventions (Kopchak et al., 2009; Babi and Momot, 2000).
To date, almost no one denies that purulent-septic complications are an absolute indication for surgical treatment. In contrast, the need for surgery in nonbacterial necrotizing pancreatitis is still unclear. Early operations in the setting of intoxication and pancreatogenic shock usually cause the death of a patient in the early postoperative period. At the same time, delayed surgical care causes purulent complications, a progression of necrotizing pancreatitis, intoxication, and multiple organ failure (Kopchak et al., 2009; Siplivy et al., 2009).
The article aims to study the clinical profile of patients with severe AP who were treated surgically during their hospital stay.
Materials and Methods
Retrospective analysis of results of treating 125 patients with severe forms of acute pancreatitis was carried out. The inclusion criterion was a severe form of acute pancreatitis associated with organ failure (cardiovascular, respiratory, and/or renal). All patients consented to participate in the study. The current study meets the criteria established by the Declaration of Helsinki.
The age of patients ranged from 19 to 90 (54.6 ± 2.3). Patients involved 80 men (64%), 45 women (36%), respectively. The minimum age for men was 19, the maximum age was 86, for women - 24 and 90, respectively. 2 (1.6%) patients were under the age of 20, 42 (33.6%) patients were between 21 and 40, 35 (28%) patients – between 41 and 60, 31 (24.8%) patients -between 61 and 75, 15 (12%) patients were at the age of 76 and older.
Causative factors for development of severe forms of acute pancreatitis involved: 41 (32.8%) patients showed alimentary; 31 (24.8%) patients - alcohol ingestion; 49 (39.2%) patients - gallstone disease; in 1 (0.8%) patient, a pancreatic injury caused pancreatitis; in 3 (2.4%) patients, causative factors weren’t clear.
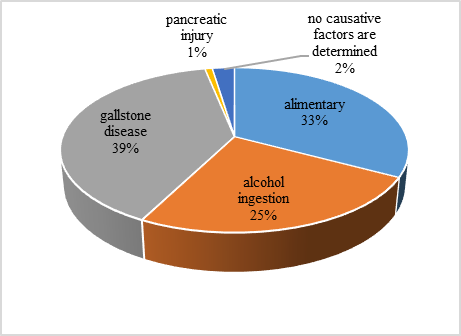
Figure 1. Causative factors for the development of severe forms of acute pancreatitis
The average time from the disease onset to the admittance of patients at a surgical hospital was 5.2 days.
Severe forms of acute pancreatitis include acute interstitial pancreatitis and nonbacterial necrotizing pancreatitis (NP) with enzymatic peritonitis and/or acute aseptic peripancreatic fluid accumulation and infected necrotizing pancreatitis regardless of extra and/or intraperitoneal complication development (Foster et al., 2016).
Based on this classification, patients are divided as follows: acute interstitial pancreatitis with enzymatic peritonitis and acute aseptic peripancreatic fluid accumulation - diagnosed in 18 patients (13.95%), nonbacterial necrotizing pancreatitis with enzymatic peritonitis and acute aseptic peripancreatic fluid accumulation - diagnosed in 27 patients (20 95%), infected necrotizing pancreatitis - diagnosed in 80 patients (65,1%). The group of patients infected with necrotizing pancreatitis included patients in whom a suppurative focus in pancreatic tissue, retroperitoneal tissue, or either in the pancreas or in retroperitoneal tissue was found during the surgery.
Patients were divided into 2 groups: 80 (64%) patients with retroperitoneal tissue damage and 45 (36%) patients without it. The extent of retroperitoneal tissue damage was determined according to the classification suggested by A.D. Tolstoy et al., 1999: multiple peripancreatic tissue abscess was detected in 2 patients, confluent necrotic phlegmon - in 25 patients, confluent necrotic phlegmon and one leakage - in 19 patients, injury of several retroperitoneal tissue areas - in 14 patients.
Another group was added into this classification - retroperitoneal tissue edema (20 patients), which can be considered as retroperitoneal phlegmon in the infiltration stage.
In the preoperative period, all patients underwent ultrasound diagnostics. In 40 patients, computed tomography was applied in addition to the ultrasound examination. Ultrasound diagnosis and computed tomography data obtained before the surgery were compared to data obtained in the intraoperative period.
To assess the disease severity in patients at admission, before surgery and in the postoperative period (1-2, 3-4, 5-7 and 8-10th day after surgery) objectively, ASSES (Acute Sepsis Severity Evaluation Score) – a score assessing the disease severity in patients with acute sepsis – was applied (Siplivy et al., 2009).
Statistical data processing involved calculations of the arithmetic mean (M) and its error (m). The characteristics were compared using the Mann-Whitney U-test and Student's t-test. To determine the predictive accuracy of each of the indicators, the ROC (Receiver Operator Characteristic) analysis was applied along with area determination under the ROC-Curve (AUC-Area Under the Curve). Analysis Studio professional edition 6.30 and Statistica 6.0 were used for statistical analysis. A normality test was carried out using the Shapiro-Wilk test. All data were consistent with the normal distribution law. The value of Р≥0.5 was significant.
Results
In 75 (60%) patients, upon admission to the hospital, systemic inflammatory response syndrome (SIRS) was detected. Out of these, 49 patients (65.3%) were diagnosed with retroperitoneal tissue damage. SIRS criteria for these patients included: body temperature above 38°C, heart rate more than 90 beats per minute, the respiratory rate of more than 20 per minute, white blood cells more than 12 g/l, more than 10% of immature neutrophils.
When admitted at the hospital, the main complaint of patients was differently localized pain, which occurred in all 125 patients. Upper abdomen pain was diagnosed in 100 (80%) patients, lower abdomen pain - in 3 (2.4%) patients, pain throughout the abdomen - in 22 (17.6%) patients. Nausea, vomiting was found in 77 (61.6%) patients. Hyperthermia, tachycardia, tachypnea was observed in 75 (60%) patients; stool and gas retention, bloating - in 93 (74.4%) patients; ochrodermia and icteric mucous membranes - in 16 (12.8%) patients.
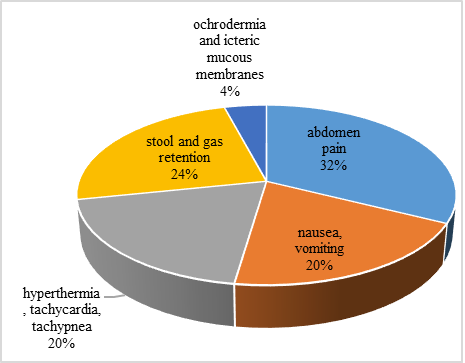
Figure 2. Main complaints of patients
Both pathologies in the pancreatic tissue directly and pathologies in the peripancreatic area were taken into account when carrying out the ultrasound examination. According to the data obtained from the ultrasound examination, pancreatic edema (pancreas is enlarged, diffusely inhomogeneous, echoicity is moderately increased, without hypoechoic foci) were detected in 15 patients with severe forms of acute pancreatitis; pancreas destruction (hypoechoic foci revealed) - in 103 patients. It should be noted that in 7 (5.6%) patients with severe forms of acute pancreatitis, no pathologies in pancreatic tissue were found during the ultrasound examination. Insufficient pancreas imaging in these patients was due to a large number of intestinal gases and altered pancreatic echoicity, which approached the structure of retroperitoneal tissue (Siplivy et al., 2009; Konkova, 2005).
Pathologies in the peripancreatic area involved omentobursitis detected in 36 patients (28.8%), pancreatogenic abscess detected in 19 (15.2%), retroperitoneal phlegmon was imaged in 65 patients (52%). In 14 patients (11.2%), peripancreatic infiltrate was detected (Figure 3). Out of the 40 patients, who were examined with computed tomography in addition to ultrasound, 32 showed retroperitoneal tissue damage, which corresponded to groups C, D, E according to the Baltazar classification (Brown et al., 2020) (multiple abscesses - 1 patient, retroperitoneal tissue infiltration - 2 patients, confluent necrotic phlegmon - 9 patients, confluent necrotic phlegmon and one leakage - 13 patients, damage in several retroperitoneal tissue areas - 7 patients). In 8 patients, signs of acute pancreatitis with no retroperitoneal tissue damage (interstitial pancreatitis - 1 patient, necrotizing pancreatitis - 7 patients) were revealed during computed tomography. 1 patient was assigned to group A, 7 patients to group B - according to the Baltazar classification.
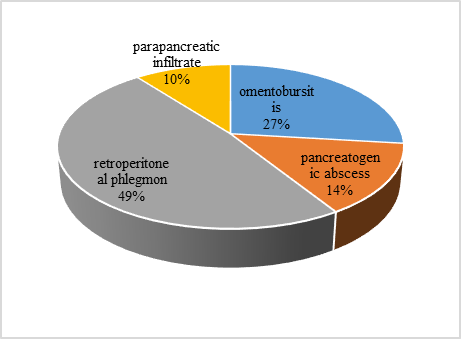
Figure 3. Pathologies in the peripancreatic area
Immediately after admission at the hospital, patients were given comprehensive conservative therapy, which was aimed to level off the water-electrolyte balance (dimephosphone, sodium chloride), to block pancreatic secretion (aprotinin), to block nociceptive pulsation in the central nervous system (CNS), to block cytokine aggression (cardiac glycosides), to prevent DIC syndrome development, to prevent and treat of stress digestive tract disease (aluminum sucrose sulphate), as well as to prevent and treat an infection.
All patients were operated on. Surgery indications included: peritonitis clinical picture in 117 patients (93.6%), arosive vessel bleeding in the necrotizing and sequestrum area in 4 patients (3.2%), jaundice growth in 4 patients (3.2%). 83 (66.4%) patients were operated on in the first 24 hours after admission at the hospital, 13 (10.4%) patients were operated on in the first 48-72 hours. 29 (23.2%) patients were operated on later than 72 hours after admission at the hospital (Table 1).
Table 1. Operation time
|
Time |
% |
|
In the first 24 hours after admission at the hospital |
66,4 |
|
In the first 48-72 hours after admission at the hospital |
10,4 |
|
Later than 72 hours after admission at the hospital |
23,2 |
Omental sac and abdominal cavity were drained in 45 (36%) patients. This operation was performed in patients with no retroperitoneal tissue damage.
Intraoperative retroperitoneal tissue damages were detected in 80 (64%) patients. If retroperitoneal tissue edema was detected, the abdominal membrane was dissected along the upper and lower pancreas edge (20 (16%) patients). Retroperitoneal phlegmon was found in 58 (46.4%) patients, and 14 (11.2%) patients had total phlegmon.
In 2 (1.6%) patients, multiple peripancreatic abscesses were found during surgery. In these cases, retroperitoneal tissue was opened and drained, omental sac and abdominal cavity were drained. In 49 (39.2%) patients with hyperbilirubinemia above 50 μmol/L, the operation also included cholecystostomy (18 patients) or cholecystectomy (31 patients), which in 23 patients was combined with external common bile duct draining. Patients had only external biliary tract draining.
Operational pancreas interventions were completed applying through omental sac draining. In total or subtotal NP, a through-draining technique was used for further continuous-flow dialysis. Retroperitoneal space draining was carried out mainly through separate lumbotomy approaches.
15 (12%) patients were treated with therapeutic relaparotomy within 2 to 15 days after the first surgical intervention. The reasons for relaparotomy were distributed as follows: 7 (46.7%) patients were treated with laparoscopy due to peritonitis, 6 (40%) patients had their omental sac, abdominal cavity and/or retroperitoneal space abscess opened and drained, in 1 (6, 65%) patient, relaparotomy was associated with outflow of bile from the cystic duct remnant and in 1 (6.65%) patient, arosive vessel bleeding in the necrotizing and sequestrum area was arrested.
It should be noted that one patient was treated with 3 laparoscopy surgeries for long-lasting peritonitis. Out of 15 patients who were treated with relaparotomy, 14 (93.3%) were diagnosed with infected NP during the first operation, and 11 (73.3%) showed disease retroperitoneal tissue (Fig. 4). Out of 125 patients, 91 (72.8%) survived, 34 (27.2%) died. Infected pancreatic necrosis was detected in 30 (88.2%) of those patients who died during surgery. In 4 (11.8%) patients, aseptic pancreas destruction was detected. It should be noted that, according to intraoperative or pathologic autopsy data, all deceased had subtotal or total pancreatic necrosis.
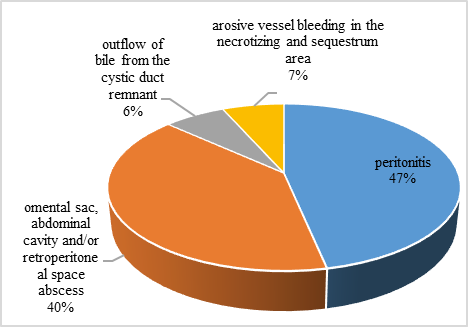
Figure 4. Reasons for relaparotomy treatment
In 26 (76.5%) of those patients who died affected by pancreatic necrosis, retroperitoneal tissue disease was detected. Thus, in 22 patients, septic retroperitoneal tissue phlegmon was detected, and retroperitoneal tissue edema associated with aseptic pancreatic necrosis was detected in 4 patients. Based on the pattern of retroperitoneal tissue damage in the deceased, confluent necrotic phlegmon was detected in 10 cases (29.4%), confluent necrotic phlegmon with leakage - in 8 cases (23.5%), several affected areas of retroperitoneal tissue - in 4 patients (11.7%) (Fig. 5).
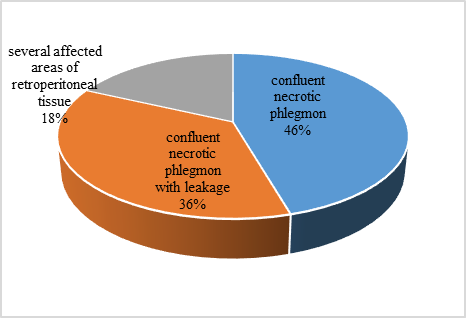
Figure 5. Retroperitoneal tissue disease pattern
Among the causes of death, intoxication dominated - 23 (67.7%) of the deceased, followed by acute cardiovascular insufficiency - 6 deceased (17.7%). Pulmonary edema was detected in 2 (5.9%) decreased, cerebral edema in 1 deceased (2.9%), hemorrhagic shock - in 1 deceased (2.9%), multiple organ failure - in 1 deceased (2.9%) (Fig. 6).
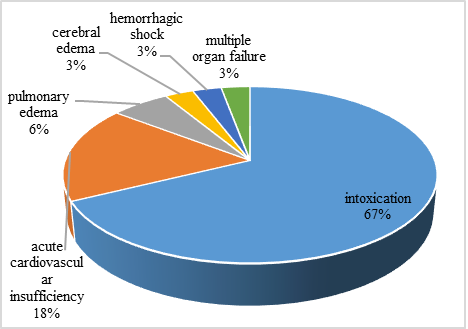
Figure 6. Causes of patients' death
ASSES scale value analysis carried out during treatment showed statistically significant differences in patients, survived and dead at all follow-up periods, the deceased showing higher scores. Thus, upon admission at the hospital, total ASSES scores for the deceased was 14.17 ± 0.92, and for patients who survived - 10.19 ± 0.64.
The highest ASSES scale values in both survived and dead patients were found on the 1st-2nd day after surgery. The increase in scores in patients survived on the 1st-2nd day after surgery which reached a record of up to 12.60 ± 0.52 compared to the pre-operative values of 11.74 ± 0.77 is not statistically significant (p = 0,068).
In the postoperative period, there was a gradual decrease in values in survived patients: down to 10.00 ± 0.65 on the 3rd-4th day after surgery (differences between the values determined in patients who survived on the 1st-2nd day and the 3rd-4th day after surgery are statistically significant - p < 0,001). On the 5th-7th day, the value decreased to 9.40 ± 0.07 (differences are statistically significant compared to the 3rd-4th day - p = 0,003).
In the deceased, the increase in ASSES scores on the 1st-2nd day of the postoperative period to 17.92 ± 0.78 compared with the scores 15.05 ± 1.00 identified before surgery is statistically insignificant (p = 0,061). A subsequent slight decrease in scores down to 17.44 ± 1.05 on the 3rd-4th day, down to 16.00 ± 1.04 on the 5th-7th day and down to 12.83 ± 1.70 on the 8th-10th day is also not statistically significant.
The number of points was determined for the ASSES to score that most accurately divide the groups of patients with a low and high lethality prediction: upon admission and before surgery - 13 points, on the 1st-2nd day and 3rd-4th day after surgery - not higher than 16 points.
If the total ASSES scale points upon admission at the hospital are not higher than 13, the lethality rate was 22.22%, higher than 13 - 65%. If the total points before the operation were not higher than 13, the lethality rate was 19.44%, higher than 13 - 51.85%.
If the total points on the 1st-2nd day after surgery were not higher than 16, lethality was 8.96%, if it was higher than 16 - 56.25%. On the 3rd-4th day after the operation, if the total points were 16 and lower, lethality reached 11.11%, higher than 16 - 70.59%.
Conclusion
References
Babi Y.S., Momot N., Savchenko A.A. (2000). Computed tomography in diagnosing acute pancreatitis forms. Ukrainian radiology journal;1:34-37.
Brown A., Goel A. et al. Balthazar score // Radiopaedia. – URL: https://radiopaedia.org/articles/balthazar-score (date of access: 14.05.2020)
Foster, B. R., Jensen, K. K., Bakis, G., Shaaban, A. M., & Coakley, F. V. (2016). Revised Atlanta classification for acute pancreatitis: a pictorial essay. Radiographics, 36(3), 675-687.
Haghighi-Morad, M., Nadi, K. & Rampisheh, Z. (2018). An observation study on the correlation between gallstone disease with non-alcoholic fatty liver disease in Iranian population as a metabolic syndrome: review of radiologic and clinical characteristics. Journal of Advanced Pharmacy Education & Research, 8(S2), 30-33.
Kanjikar, A. P. (2019). On Anti-Diabetic Potential of Phyto-nanoparticles Comparison with Hormonal Therapy and Medicinal Plants. International Journal of Pharmaceutical and Phytopharmacological Research, 9(1), 103-111.
Konkova M.V. (2005). Diagnostic and interventional sonography in emergency abdominal surgery. Donetsk, 104-118.
Kopchak V.N., Khomyak I.V., Kopchak K.V. et al. (2009). Acute necrotizing pancreatitis: current approaches to surgical treatment. Kharkov Surgical School. 3.1 (35):78-80.
Leppäniemi, A., Tolonen, M., Tarasconi, A., Segovia-Lohse, H., Gamberini, E., Kirkpatrick, A. W., ... & van Goor, H. (2019). 2019 WSES guidelines for the management of severe acute pancreatitis. World Journal of Emergency Surgery, 14(1), 27.
Mohamed, N. R. & Badr, T. M. (2019). Protective Role of Chicory Leaves Extract against Gamma Radiation-Induced Bone Loss and Down-expression of Osteocalcin Gene in Albino Female Rats. International Journal of Pharmaceutical and Phytopharmacological Research, 9(2), 69-82.
Nazarenko P. M., Nazarenko D. P., Alekhin S. A., Belikov L. N. (2019). Peptic ulcer, acute pancreatitis, portal hypertension: selected lecture course on abdominal surgery. FSBEI of Higher Education Kursk State Medical University of the Ministry of Health of the Russian Federation, Department of Surgical Diseases No. 2. Kursk: Kursk State Medical University.
Siplivy V.A., Dronov A.I., Kon E. et al. (2009). Assessment of disease severity of a surgical patient. Moscow,77-100.
Tolstoi, A. D., Panov, V. P., & Krasnorogov, V. B. (2003). Parapankreatit. Etiologiia, patogenez, diagnostika, lechenie [Parapancreatitis. Etiology, pathogenesis, diagnosis, treatment]. St. Petersburg: Iasnyi svet Publ., 256 p.

